|
 |
- Search
| Neonatal Med > Volume 28(2); 2021 > Article |
|
This article has been retracted. See "Intussusception and Jejunal Atresia Caused by an Ectopic Pancreas in a Newborn" on page 72.
This article has been retracted. See "Retraction Notice: Intussusception and Jejunal Atresia Caused by an Ectopic Pancreas in a Newborn" on page 55.
This article has been retracted. See "Retraction Notice: Intussusception and Jejunal Atresia Caused by an Ectopic Pancreas in a Newborn" on page 55.
This retracted the article "Intussusception and Jejunal Atresia Caused by an Ectopic Pancreas in a Newborn" on page 72.
Abstract
Ectopic pancreas is defined as an abnormally located pancreatic tissue not sufficiently connected with the normal pancreas, which rarely occurs in neonates. To our knowledge, only a few cases of ectopic pancreas have been reported in newborns in South Korea. We report a case of ectopic pancreas as the cause of intussusception and jejunal atresia in a newborn. This clinical association is extremely rare, and this is the first report in South Korea.
An ectopic pancreas is an abnormally located pancreatic tissue without anatomical or vascular continuity with the normal pancreas when examined histologically [1]. It has an overall prevalence of 1% to 13% [2], but rarely affects neonates. An ectopic pancreas is most frequently located in the following organs: the gastrointestinal tract (25% to 38%), duodenum (17% to 36%), and jejunum (15% to 21%). It may also be present in the liver, Meckel’s diverticulum, navel, spleen, and fallopian tubes [3]. It is mostly asymptomatic when no complications occur and thereby is often only detected spontaneously during surgery or imaging examinations. However, in some cases with complications, an ectopic pancreas may present with pancreatitis, pancreatic pseudocyst, malignant transformation, gastrointestinal hemorrhage or atresia, and intussusception. To our knowledge, only three cases of ectopic pancreas have been reported in newborns in South Korea, including a report of ectopic pancreas with gastroschisis in 1983 [4], a patient with an annular pancreas with duodenal obstruction in 1992 [5], and a case of duodenal obstruction due to ectopic pancreas in 1996 [6]. We report a case of a neonate admitted to our institution due to bilious vomiting on the second day of life (DOL), who was diagnosed with jejunal atresia with intussusception due to an ectopic pancreas.
A 3,320 g female infant was born at 39 gestational weeks via normal spontaneous vaginal delivery. Amniotic fluid was meconium- stained, without other clinical symptoms noted. Apgar scores were 9 at 1 minute and 10 at 5 minutes. The first urination and defecation were observed on DOL1. She was transferred to our neonatal intensive care unit due to bilious vomiting on DOL2. No abnormalities or risk factors were detected during the prenatal examination, maternal history, or family history. On physical examination, the infant showed mild abdominal distension and reduced bowel sounds with normal vital signs. No bloody stools were noted. Laboratory test results were within normal limits. Abdominal radiography showed dilated small bowel loops and a gasless rectum, indicating the possibility of intestinal obstruction (Figure 1). On abdominal ultrasonography, intussusception was suspected in the small bowel (Figure 2). A lower gastrointestinal contrast study revealed no significant abnormalities. No evidence of hypertrophic pyloric stenosis, duodenal stenosis, or intestinal malrotation was observed in the upper gastrointestinal contrast examination. Exploratory laparotomy was performed, and an approximately 30×20-mm hemorrhagic mass, located at the inner mucosa 75 cm distal to the ligament of Treitz, was detected. This mass resulted in jejunojejunal intussusception (Figure 3A), for which manual reduction was performed without difficulty. In addition, the jejunum is obstructed by an intact membrane composed of mucosa and submucosa proximal to the mass. The muscularis and serosa remained intact, resulting in the absence of discontinuity in the bowel (jejunal atresia type I) (Figure 3B). As no other abnormalities were found in other areas of the gastrointestinal tract, the atretic segment of approximately 5 cm was resected with end-to-end anastomosis. Histopathological analysis of the resected mass showed a hemorrhagic lesion on the jejunal wall with pancreatic ducts of varying sizes, and in some cases, squamous metaplasia was observed. An additional observation of the atrophic pancreatic acinus around the pancreatic ducts led to the diagnosis of an ectopic pancreas (Figure 4).
Enteral feeding was started 5 days postoperatively, and the infant was discharged on day 29 after admission. During the 2-month follow-up, the infant showed normal growth and development without other abnormalities, such as vomiting or abdominal distension.
An ectopic pancreas is a pancreatic tissue with insufficient vascular and anatomical structures. It is a rare form of congenital malformation first reported by Shultz in 1729 [7]. The first histological report was made by Klob in 1895 [8]. Sohn et al. [9] reported a case of a jejunal ectopic pancreas in 1967. Ectopic pancreas in infants has been sparsely reported since Min et al.’s first report in 1971 [10]. To our knowledge, only three relevant case reports in newborn infants have been found [4-6].
The majority of ectopic pancreas (90%) is located in the stomach, duodenum, jejunum, and other abdominal organs, which are often coincidentally detected during an open surgery [3]. Its symptoms vary according to the amount of mechanical pressure on the intestines, which leads to acute inflammation of the gastrointestinal tract. It is often asymptomatic in neonates [11]. An ectopic pancreas may also lead to complications, such as atresia, hemorrhage, inflammation, and malignant transformation [12]. We report an extremely rare case of jejunal atresia with intussusception caused by an ectopic pancreas that presented with bilious vomiting on DOL2. However, even in asymptomatic cases, an incidentally detected ectopic pancreas should be removed entirely through wedge resection to prevent any risk of complications. Furthermore, in neonates with an ectopic pancreas, the diagnosis of hypertrophic pyloric stenosis, duodenal stenosis or atresia, and intestinal malrotation should be ruled out. In the present case, abdominal ultrasonography and contrast examinations were performed to rule out upper gastrointestinal atresia.
Intussusception refers to the invagination of the bowel segment into the distal part of the bowel and is the most common cause of intestinal atresia among infants [13]. It rarely occurs in neonates, with only 0.1% of neonates diagnosed within 2 months of birth, according to a recent study conducted in South Korea [13]. As the cause of intussusception remains unknown in most infants (75%), a Meckel diverticulum, polyp, duplication cyst, tumor, hematoma, or vascular malformation may act as a lead point for intussusception [14]. Jejunal atresia, accounting for 20% of all intestinal atresia, results from ischemic necrosis of the fetal intestine due to vascular disruption. Segmental or midgut volvulus, intussusception, internal hernia, and interruption of the segmental mesenteric blood supply may cause vascular disruption [15,16]. In general, a more proximal vascular disruption leads to a more extensive bowel defect. The patient presented in this case report had a rare case of intussusception with jejunal atresia (type I) caused by ectopic pancreas as the leading point.
The exact embryology of ectopic pancreas remains unknown, although various theories have been presented. Skandalakis et al. [17] suggested that this may be due to the atypical metaplasia of multipotent endodermal cells in the primitive intestine. Conversely, Armstrong et al. [18] suggested that the pathology occurred during rotation and combination of the dorsal and ventral pancreatic buds. Furthermore, Abel et al. [19] suggested that an ectopic pancreas is caused by abnormal involution of the vitelline-enteric duct in relation to the gastric mucosa. An ectopic pancreas can be divided into four pathological types: type I, only a specific pancreatic tissue is present; type II, only the pancreatic duct is present; type III, only the acinar tissue is present; and type IV, only the islet cells are included [20]. The case presented in this study was classified as a type I ectopic pancreas due to the development of pancreatic ducts of varying sizes and the presence of certain types of squamous metaplasia and atrophic pancreatic acinus around the pancreatic ducts.
This study reported the case of a newborn infant admitted to our institution due to bilious vomiting who was diagnosed with a rare case of small intestinal intussusception with complete jejunal atresia caused by an ectopic pancreas. In neonates with symptoms of intestinal obstruction, various possibilities should be considered in an effort toward active differential diagnosis. Abdominal ultrasonography and gastrointestinal contrast examinations are useful diagnostic tests for obtaining additional information. Exploratory laparotomy can be performed in severe symptomatic cases or when a differential diagnosis is required.
ARTICLE INFORMATION
Figure 3.
(A) Exploratory laparotomy reveals the presence of jejunojejunal intussusception (arrow). (B) A hemorrhagic mass and jejunal atresia are found in the distal jejunum (arrow).
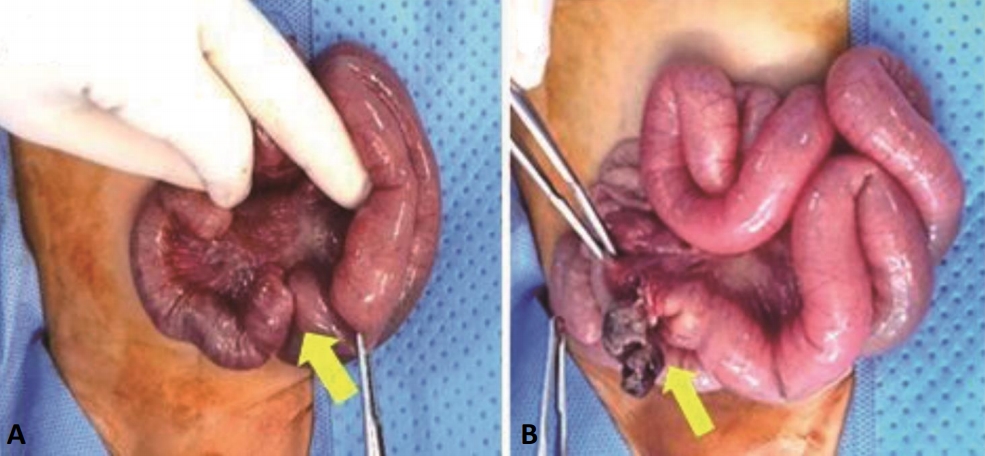
Figure 4.
(A) A hemorrhagic mass-like lesion is detected on the jejunal wall (black arrow). Squamous metaplasia is also observed (H&E stain, ×0.5). (B) Histological examination of the jejunal mass demonstrates the presence of pancreatic ducts (yellow arrows) (H&E stain, ×5.0). (C) The tissue section reveals a pancreatic acinus with a heterotopic pancreas (yellow arrows) (H&E stain, ×5.0).

REFERENCES
1. Hirasaki S, Kubo M, Inoue A, Miyake Y, Oshiro H. Jejunal small ectopic pancreas developing into jejunojejunal intussusception: a rare cause of ileus. World J Gastroenterol 2009;15:3954–6.



2. Rezvani M, Menias C, Sandrasegaran K, Olpin JD, Elsayes KM, Shaaban AM. Heterotopic pancreas: histopathologic features, imaging findings, and complications. Radiographics 2017;37:484–99.


3. Ormarsson OT, Gudmundsdottir I, Marvik R. Diagnosis and treatment of gastric heterotopic pancreas. World J Surg 2006;30:1682–9.


4. Yoon HS, Hyun MS, Hahn JH, Ahn SW, Yang JW. One case of ectopic pancreatic tissue with gastroschisis. J Korean Pediatr Soc 1983;26:1009–12.
5. Choi JS, Park BW, Min JS. Heterotopic pancreas. Korean J Gastroenterol 1992;24:1403–10.
6. Han HS, Han SJ, Lee HJ, Park WI, Lee KJ, Ryu BY. A case of duodenal obstruction in the newborn due to ectopic pancreas. Inkan Kwahak 1996;20:53–6.
7. Kilius A, Samalavicius NE, Danys D, Zaldokas G, Seinin D. Asymptomatic heterotopic pancreas in Meckel's diverticulum: a case report and review of the literature. J Med Case Rep 2015;9:108.



8. Gokhale UA, Nanda A, Pillai R, Al-Layla D. Heterotopic pancreas in the stomach: a case report and a brief review of the literature. JOP 2010;11:255–7.

9. Sohn KH, Kim YB, Chi JG. Heterotopic pancreas: a case report. J Korean Surg Soc 1967;9:793–801.
10. Min BJ, Chung CK, Hwang EH. Intussusception due to heterotopic pancreas. J Korean Surg Soc 1971;13:49–53.
11. Ueno S, Ishida H, Hayashi A, Kamagata S, Morikawa M. Heterotopic pancreas as a rare cause of gastrointestinal hemorrhage in the newborn: report of a case. Surg Today 1993;23:269–72.


12. Fam S, O'Briain DS, Borger JA. Ectopic pancreas with acute inflammation. J Pediatr Surg 1982;17:86–7.


13. Jo S, Lim IS, Chae SA, Yun SW, Lee NM, Kim SY, et al. Characteristics of intussusception among children in Korea: a nationwide epidemiological study. BMC Pediatr 2019;19:211.



14. Lin XK, Xia QZ, Huang XZ, Han YJ, He GR, Zheng N. Clinical characteristics of intussusception secondary to pathologic lead points in children: a single-center experience with 65 cases. Pediatr Surg Int 2017;33:793–7.


15. Kao KJ, Fleischer R, Bradford WD, Woodard BH. Multiple congenital septal atresias of the intestine: histomorphologic and pathogenetic implications. Pediatr Pathol 1983;1:443–8.


16. Grosfeld JL, Ballantine TV, Shoemaker R. Operative mangement of intestinal atresia and stenosis based on pathologic findings. J Pediatr Surg 1979;14:368–75.

17. Skandalakis LJ, Rowe JS Jr, Gray SW, Skandalakis JE. Surgical embryology and anatomy of the pancreas. Surg Clin North Am 1993;73:661–97.


18. Armstrong CP, King PM, Dixon JM, Macleod IB. The clinical significance of heterotopic pancreas in the gastrointestinal tract. Br J Surg 1981;68:384–7.


19. Abel R, Keen CE, Bingham JB, Maynard J, Agrawal MR, Ramachandra S. Heterotopic pancreas as lead point in intussusception: new variant of vitellointestinal tract malformation. Pediatr Dev Pathol 1999;2:367–70.


20. Trandafir LM, Aprodu SG, Mihaila D, Anton Paduraru DT, Butnariu L, Straticiuc Ciongradi IC. Ectopic jejunal pancreas and congenital duodenal stenosis in a newborn patient: an unusual association. Rom J Morphol Embryol 2014;55(2 Suppl):707–10.