|
 |
- Search
| Neonatal Med > Volume 30(2); 2023 > Article |
|
This article has been corrected. See Neonatal Med. 2023 Aug 31; 30(3): 88.
Abstract
Purpose
Infants in the neonatal intensive care unit (NICU) often show cardiorespiratory deterioration during gavage feeding. We aimed to determine whether slow infusion intermittent feeding (SIIF) can reduce respiratory deterioration during gavage feeding in preterm infants in the NICU.
Methods
Data on preterm infants whose gavage feeding method was changed to SIIF (1-hour infusion with an infusion pump and 2-hour rest within a 3-hour interval) from bolus gravity feeding (2- or 3-hour interval) due to feeding-associated cardiorespiratory deterioration were retrospectively reviewed. A significant cardiorespiratory event was defined as a saturation level below 80% or heart rate below 80 bpm. We compared the frequency of cardiorespiratory events and the level of respiratory support 24 hours before and after the application of SIIF.
Results
A total of 34 infants were enrolled and analyzed. The total frequency of desaturation or bradycardia significantly decreased after SIIF application (8.94 vs. 5.03, P=0.001). The frequency of feeding-related bradycardia and desaturation also significantly decreased (4.15 vs. 1.68, P=0.008). Out of 34 patients, 11 (32.4%) had a decreased level of ventilator support within 1 day after SIIF. The respiratory severity scores of the 10 patients who received invasive ventilator support decreased significantly after SIIF (5.24 vs. 4.59, P=0.032).
Early enteral feeding is the current standard protocol for preterm infants, as enteral nutrition has significant nutritional and non-nutritional benefits compared with parenteral nutrition [1]. To achieve enteral nutrition, the use of orogastric or nasogastric tubes is necessary for preterm infants born before 32 weeks of pregnancy because of underdeveloped suck-swallow-breath coordination [2]. However, even with gavage tubes enteral feeding is difficult for preterm infants, especially in addition to respiratory support.
Feeding-related cardiorespiratory symptoms are prevalent among preterm infants. Studies on feeding-associated cardiorespiratory events have identified suitable enteral feeding methods; however, no consensus has been reached on a feeding method for preterm infants with feeding-associated cardiorespiratory deterioration. As such, the feeding method for each patient is based on the judgment of the clinician.
In our center, slow infusion intermittent feeding (SIIF) was applied to reduce feeding-associated cardiorespiratory events, which consisted of 1 hour of feeding with an infusion pump followed by 2 hours of rest. This study aimed to determine whether SIIF could reduce cardiorespiratory deterioration during gavage feeding in preterm infants.
We conducted a retrospective cohort study between January 2019 and March 2023, designed to enroll SIIF-fed preterm infants with birth weights <1,500 g or gestational ages <32 weeks with gavage feeding-associated respiratory deterioration. Infants with sepsis, patent ductus arteriosus requiring treatment, necrotizing enterocolitis, or any type of surgery that could affect cardiorespiratory events at the time of SIIF initiation were excluded.
Intermittent 3-hour bolus gravity feeding is the first-line standard feeding technique for all preterm infants admitted to the neonatal intensive care unit (NICU) at Seoul National University Bundang Hospital. If feeding-related symptoms occurred after achieving an enteral feed amount of ≥100 mL/kg/day, intermittent 3-hour interval bolus gravity feeding was changed to 2-hour interval bolus feeding to decrease the amount given at each feeding. If feeding-related cardiorespiratory events persisted, then SIIF was performed. SIIF consisted of feeding with an infusion pump for 1 hour, followed by 2 hours of rest. During SIIF, an infusion pump and warmer were used to feed at a constant speed and temperature for over 1 hour. In addition, an infusion pump was installed vertically to minimize the loss of sinking nutrients. When feeding-related cardiorespiratory events and ventilator support levels were significantly reduced, we changed SIIF to the standard intermittent 3-hour interval bolus feeding while maintaining the feed delivered at once.
Demographic and clinical data were retrospectively collected from electronic medical records. Cardiorespiratory events, level of respiratory support, and respiratory severity score (RSS), which is a product of the mean airway pressure multiplied by the fractional inspiration of oxygen (FiO2) [3], were compared 24 hours before and after the application of SIIF. Data on the following morbidities were also collected: bronchopulmonary dysplasia (BPD), which was defined using the National Institute of Child Health criteria for BPD and graded as mild, moderate, or severe according to the FiO2 or positive pressure ventilation; surfactant use for respiratory distress syndrome; Bell’s classification NEC ≥stage 2; retinopathy of prematurity; and culture-proven lateonset sepsis.
A significant cardiorespiratory event was defined as a saturation level below 80% or heart rate below 80 bpm. Feeding-related cardiorespiratory events were defined as those that occurred during or within 30 minutes of feeding. Cardiorespiratory monitoring and pulse oximetry were performed in all patients. In our NICU, we used a Philips IntelliVue MX800 monitor that provided continuous oxycardiogram data with a beat-to-beat heart rate. Saturation of partial pressure oxygen (SpO2) was monitored using disposable pulse oximetry sensors (Nellcor with OxiMax), and heart rate was measured using a 3-lead electrocardiogram sensor (Ambu BlueSensor BRS). If bradycardia occurred, or the saturation level fell below the cutoff, the cardiorespiratory monitor alarm switched off immediately. The nurse assigned to each infant checked the bedside monitor in real time when the alarm turned off and documented each event, including the lowest heart rate, lowest saturation, and relationship with feeding if the event occurred during or within 30 minutes after feeding.
A total of 376 preterm infants with birth weights <1,500 g or gestational ages <32 weeks were born between January 2019 and March 2023. Among them, 34 patients whose feeding method was changed to SIIF were enrolled in this study. The study population demographics and clinical characteristics are presented in Table 1. The mean gestational age was 26.4±1.9 weeks and mean birth weight was 857.7±265.1 g. The mean postmenstrual age at the time of SIIF application was 30.1±1.9 weeks, and the duration of SIIF was 25.4±14.0 days. The mean postmenstrual age at the end of SIIF was 33.6±2.3 weeks.
Figure 1A shows the differences in the frequency of cardiorespiratory events before and after SIIF. The total frequency of bradycardia or desaturation was significantly decreased after SIIF (8.94±8.29 vs. 5.03±6.24, P=0.001). The frequency of feedingrelated bradycardia or desaturation was also significantly decreased (4.15±5.52 vs. 1.68±2.27, P=0.008), as shown in Figure 1B.
For patients receiving invasive ventilation, we used the RSS to determine the level of support. The RSSs before and after SIIF were compared among the 10 patients who received invasive ventilator support at the time of SIIF; the results are presented in Figure 2. The RSS significantly decreased after SIIF (5.24±1.05 vs. 4.59±0.95, P=0.032). In patients receiving noninvasive ventilator support at the time of SIIF application, the level of respiratory support was considered to have increased/decreased when either FiO2 or positive end expiratory pressure were increased or decreased. Out of 34 patients, respiratory support was reduced in 11 (32.4%), maintained in 16 (47%), and increased in seven (20.6%) within 1 day after SIIF initiation.
To date, there is no consensus regarding the optimal feeding method for preterm infants with feeding-related cardiorespiratory deterioration. A Cochrane review and meta-analysis of randomized controlled trials found no significant differences in the duration of hospitalization, duration of parental feeding, weight gain, and incidence of NEC between continuous and bolus feeding in preterm infants with low birth weight [4,5].
Both intermittent and continuous bolus feeding have advantages and disadvantages. Bolus feeding is a physiological method that promotes the circadian rhythm of intestinal hormones and postprandial rhythms of ghrelin and insulin release in response to nutrition [6]. Recent studies comparing bolus feeding and continuous feeding in a newborn piglet model found that intermittent bolus feeding promotes greater lean growth and protein anabolism and enhances protein synthesis [7,8]. However, several investigators have demonstrated that 24-hour continuous feeding has several advantages over bolus feeding, especially in critically ill patients [9,10]. Previous studies have shown that continuous nutrient administration is associated with fewer gastrointestinal and respiratory complications [11,12]. In preterm infants, particularly in those with a much smaller gastric capacity, bolus feedingrelated feeding intolerance and pulmonary function impairment are obvious and have been described in several studies [2,13,14]. Blondheim et al. [2] compared the effects of intermittent and continuous feeding on the pulmonary function of very low birth weight infants and found a significant decrease in tidal volume, minute ventilation, and dynamic compliance after intermittent feeding. Furthermore, infants receiving noninvasive ventilation experience an unintended influx of air through the nasopharynx, leading to marked abdominal distention, known as continuous positive airway pressure (CPAP) belly syndrome [15]. Excessive swallowed air increases the intra-abdominal pressure, which requires an increase in CPAP pressure to alleviate, resulting in a vicious cycle [15]. In addition, a large volume of enteral feeding during noninvasive ventilator support exacerbates respiratory deterioration. D'Angelo et al. [16] found that with greater levels of abdominal distension in the supine position, both the electromechanical efficiency of the diaphragm and tidal volume declined in anesthetized rabbits. A recent meta-analysis of randomized controlled trials on continuous versus intermittent bolus feeding showed that more days of continuous feeding were needed to achieve full feeding, but there were no significant differences in feeding intolerance, duration of hospitalization, duration of parental feeding, weight gain, or proven NEC [4].
In the current study, we suggest a compromised method, SIIF, which can reduce the respiratory burden of preterm infants who require respiratory support during feeding and minimize the complications of 24-hour continuous feeding by providing a 3-hour interval between feedings. We found SIIF to significantly reduce feeding-associated cardiorespiratory events and respiratory support levels.
As cardiorespiratory events in preterm infants are affected by various factors, we attempted to monitor the acute effect of SIIF by comparing events 24 hours before and after the application of SIIF. We excluded infants with other factors that could affect cardiorespiratory events beyond the feeding modality, such as clinical or culture-proven sepsis, or those within 3 days of surgical treatment. A single researcher reviewed and analyzed every cardiorespiratory event detected by bedside cardiorespiratory monitors in all patients by reviewing the electronic medical records completed by the assigned nurses. After SIIF, 27 of 34 patients (79.6%) showed a decrease in the level of ventilator support or no change in the respiratory support modality, and all patients showed significantly decreased rates of feeding-related respiratory deterioration. The levels of respiratory support increased after SIIF in seven patients who were then weaned from ventilator support or were in the middle of the BPD aggravation period. Even though respiratory support increased, five of the seven patients showed a decrease in the number of cardiorespiratory events after SIIF.
This study had some limitations. First, the measurement of cardiorespiratory events relied entirely on alarms detected by the cardiorespiratory monitor; as such, events that recovered before the alarm activated may have been missed. In addition, there are no definite criteria for feeding-related alarms in preterm infants because the gastric emptying time may be longer depending on the gestational age and other conditions. In this study, events that occurred during or within 30 minutes after 1-hour of feeding were considered feeding-related cardiorespiratory events. Because this was a single-center retrospective study with a small sample size, multicenter, larger-sample studies are needed to further evaluate the effectiveness of SIIF. To clarify the effect of SIIF, a crossover study or comparison with a control group is also required. Finally, we focused only on the respiratory-related outcomes after SIIF. Further studies on SIIF-related gastrointestinal outcomes, such as the time to reach full enteral feeding, duration of gavage feeding, and symptoms associated with feeding intolerance, are also needed.
In conclusion, SIIF significantly reduced the frequency of feeding-related cardiorespiratory events in preterm infants requiring invasive and noninvasive respiratory support. Additionally, the degree of ventilator support significantly decreased after SIIF. Therefore, SIIF may be a therapeutic option for gavage feedingassociated cardiorespiratory deterioration in preterm infants in the NICU.
ARTICLE INFORMATION
Ethical statement
Approval for this study was obtained from the Seoul National University Bundang Hospital Institutional Review Board. (IRB No. 2023-03230). Informed consent was waived by the board.
Author contributions
Conception or design: M.J.K., H.S.K., Y.H.J., C.W.C.
Acquisition, analysis, or interpretation of data: M.J.K., H.S.K., Y.H.J., C.W.C.
Drafting the work or revising: M.J.K., H.S.K., Y.H.J., C.W.C.
Final approval of the manuscript: All authors read and approved the final manuscript.
Figure 1.
Comparison of the cardiorespiratory event frequency before and after slow infusion intermittent feeding (SIIF). (A) Comparison of total cardiorespiratory event frequency before and after SIIF. Total frequency of bradycardia or desaturation was significantly decreased after the application of SIIF (8.94±8.29 vs. 5.03±6.24, P=0.001). (B) Comparison of feeding-related cardiorespiratory event frequencies before and after intermittent slow infusion feeding. The frequency of feeding-related cardiorespiratory events was significantly decreased after the application of SIIF (4.15±5.52 vs. 1.68±2.27, P=0.008). The white and grey boxes represent pre-SIIF and post-SIIF, respectively. ‘x’ indicates the mean value, the horizontal line in the middle of the box is the median value of the frequencies, and the lower and upper boundaries indicate the 25th and 75th percentiles, respectively. *P-values less than 0.05.

Figure 2.
Comparison of respiratory severity scores (RSSs) before and after slow infusion intermittent feeding (SIIF) in patients with invasive ventilator support. The RSS of the 10 patients receiving invasive ventilator support significantly decreased after SIIF (5.24 vs 4.59, P=0.032). The white and grey boxes represent pre-SIIF and post-SIIF, respectively. ‘x’ indicates the mean value, the horizontal line in the middle of the box is the median value of the frequencies and the lower and upper boundaries indicate the 25th and 75th percentiles, respectively. *P-value less than 0.05.
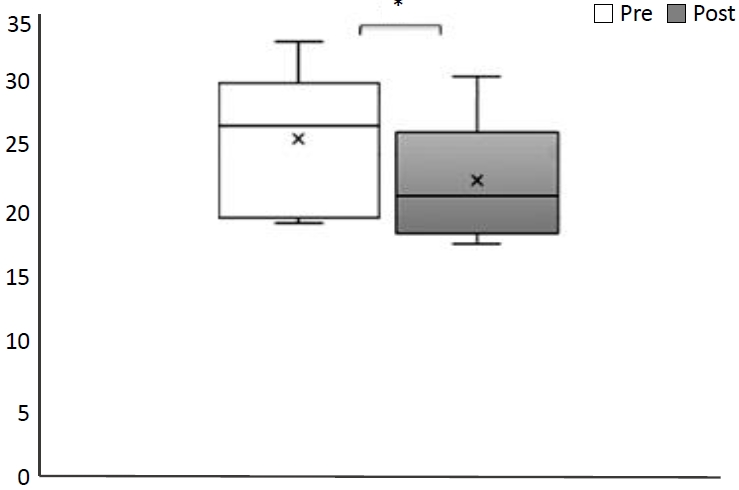
Table 1.
Basal Characteristics for the Study Population
REFERENCES
1. Thoene M, Anderson-Berry A. Early enteral feeding in preterm infants: a narrative review of the nutritional, metabolic, and developmental benefits. Nutrients 2021;13:2289.



2. Blondheim O, Abbasi S, Fox WW, Bhutani VK. Effect of enteral gavage feeding rate on pulmonary functions of very low birth weight infants. J Pediatr 1993;122(5 Pt 1): 751–5.


3. Ballard RA, Truog WE, Cnaan A, Martin RJ, Ballard PL, Merrill JD, et al. Inhaled nitric oxide in preterm infants undergoing mechanical ventilation. N Engl J Med 2006;355:343–53.


4. Wang Y, Zhu W, Luo BR. Continuous feeding versus intermittent bolus feeding for premature infants with low birth weight: a meta-analysis of randomized controlled trials. Eur J Clin Nutr 2020;74:775–83.



5. Sadrudin Premji S, Chessell L, Stewart F. Continuous nasogastric milk feeding versus intermittent bolus milk feeding for preterm infants less than 1500 grams. Cochrane Database Syst Rev 2021;6:CD001819.

6. Gonzalez JT, Dirks ML, Holwerda AM, Kouw IW, van Loon LJ. Intermittent versus continuous enteral nutrition attenuates increases in insulin and leptin during short-term bed rest. Eur J Appl Physiol 2020;120:2083–94.




7. El-Kadi SW, Boutry C, Suryawan A, Gazzaneo MC, Orellana RA, Srivastava N, et al. Intermittent bolus feeding promotes greater lean growth than continuous feeding in a neonatal piglet model. Am J Clin Nutr 2018;108:830–41.



8. Davis TA, Fiorotto ML, Suryawan A. Bolus vs. continuous feeding to optimize anabolism in neonates. Curr Opin Clin Nutr Metab Care 2015;18:102–8.



9. Hrdy O, Vrbica K, Strazevska E, Suk P, Souckova L, Stepanova R, et al. Comparison of continuous versus intermittent enteral nutrition in critically ill patients (COINN): study protocol for a randomized comparative effectiveness trial. Trials 2020;21:955.




10. Ichimaru S, Amagai T. Intermittent and bolus methods of feeding in critical care. Edited by Rajendram R, Preedy V, Patel V Diet and nutrition in critical care. Springer, 2014, pp 1–17.
11. Lee HY, Lee JK, Kim HJ, Ju DL, Lee SM, Lee J. Continuous versus intermittent enteral tube feeding for critically ill patients: a prospective, randomized controlled trial. Nutrients 2022;14:664.



12. O'Connor G, Hartfiel-Capriles Z, Saduera S. Intermittent bolus versus continuous feeding in children receiving an enteral formula with food derived ingredients: a national multicentre retrospective study. Clin Nutr ESPEN 2023;54:175–9.


13. Heldt GP. The effect of gavage feeding on the mechanics of the lung, chest wall, and diaphragm of preterm infants. Pediatr Res 1988;24:55–8.


14. Akintorin SM, Kamat M, Pildes RS, Kling P, Andes S, Hill J, et al. A prospective randomized trial of feeding methods in very low birth weight infants. Pediatrics 1997;100:E4.