Developmental Outcome of Very-Low-Birth-Weight Infants without Major Brain Injuries Based on Data from the Korean Neonatal Network: A Nationwide Cohort Study
Article information
Abstract
Purpose
As preterm infants have shown advances in survival rate, many very-low-birth-weight (VLBW) infants have shown developmental delay even without a major brain injury. Thus, the incidence of and risk factors associated with poor neurodevelopmental outcome should be evaluated.
Methods
A multicenter nationwide prospective longitudinal cohort study of VLBW infants born in South Korea between 2013 and 2015 was conducted. Poor neurodevelopmental outcome was diagnosed if the Bayley Scales of Infant and Toddler Development (BSID)-III composite score was ≤85 (cognition, language, motor). We analyzed the associations of baseline neonatal characteristics, environmental characteristics and neonatal morbidities with poor neurodevelopmental outcome.
Results
The study included 285 infants, of whom 34 (11.9%) exhibited cognition delay; 59 (20.7%), showed language delay and 32 (11.2%) showed motor delay. The mean gestational age and birth weight were 29 weeks and 1,130 g, respectively. Moderate and severe bronchopulmonary dysplasia (P=0.056) and intraventricular hemorrhage grade I (P=0.079) were marginally associated with cognition delay. Higher paternal educational level (P<0.05) was significantly associated with the language outcome. Birth weight (P<0.05) and head circumference at discharge (P<0.05) were the major predictors of motor delay.
Conclusion
The population-based nationwide cohort study shows that approximately 20% of VLBW infants without major brain injury have developmental delay. Several factors that are not directly associated with major brain injury were significantly associated with poor neurodevelopmental outcome.
INTRODUCTION
As there has been a marked improvement in the survival rates of preterm infants, their long-term developmental outcomes have become a subject of great concern. Although the survival rates of preterm infants has shown remarkable advancement, from 65.8% in the 1990s to 89.7% in 2009 [1], 30% of preterm infants showed developmental delay in South Korea [2]. In fact, 75% of preterm infants are known to have developmental disabilities around the age of 5 years [3].
Several researches have been conducted to identify the risk factors for developmental delay in preterm infants. In particular, low gestational age, especially birth at <24 weeks of gestation, has been known to have a significant effect on developmental delay. Also, it is well known that factors including low birth weight, low Apgar score, prolonged ventilator use, hypoglycemia, absent antenatal steroid, bronchopulmonary dysplasia (BPD), and retinopathy of prematurity (ROP) are significant factors of poor neurodevelopmental outcome [4-7].
Although brain magnetic resonance imaging (MRI) has been a widely accepted tool for the diagnosis of adverse neurodevelopmental outcome, there have been discrepancies between the MRI findings and clinical outcome. Woodward et al. [8] showed that 15% of preterm infants with normal findings in brain MRI showed severe neurodevelopmental delay. Also, in a subsequent study [9], preterm infants with mild brain MRI abnormality were approximately three times likely to have developmental delay at the ages of 4 to 6 years. These previous studies imply the existence of relevant factors other than major brain injury that could impact on developmental delay. However, in our knowledge, nationwide cohort studies that identified the risk factors for very-low-birth-weight (VLBW) without major brain injury have been lacking.
The Bayley Scales of Infant and Toddler Development (BSID) test was revised and reconstructed into the third edition, which includes a separation of the mental developmental index into the cognitive and receptive and expressive language scales. Compared with the second edition, BSID-III provides advantage on the detailed evaluation of infants’ developmental status as it is newly revised in 20 years to reflect the latest trends in developmental research [10]. From our knowledge, the neurodevelopmental outcome of VLBW infants using the BSID-III test has not been widely studied in South Korea.
The present study aimed to describe the incidence of the developmental outcome of VLBW infants without major brain injury. Also, using the nationwide database from the Korean Neonatal Network (KNN), the study aimed to establish the risk factors for the poor neurodevelopmental outcome.
MATERIALS AND METHODS
1. Study population
The study is a prospective longitudinal cohort study with VLBW infants enrolled in the KNN. The KNN is an ongoing web-based nationwide registry database participated by 69 hospitals across South Korea [11,12]. The registry includes approximately 70% of all VLBW infants born in South Korea. The registry database collects not only prenatal and postnatal data but also post-discharge data, including the results of the BSID test at corrected ages of 18 to 24 months. Written informed consent was obtained from the parents upon enrollment at each participating hospital. From the KNN registry, we included VLBW infants who were born between January 2013 and December 2015 with birth weights of <1,500 g and underwent the BSID-III test at corrected ages of 18 to 24 months. The exclusion criteria were VLBW infants with major congenital malformations including genetic anomalies and malformation of a major organ system. VLBW infants with seizure and periventricular leukomalacia (PVL) and intraventricular hemorrhage (IVH) grade II or higher were also excluded.
2. Neonatal variables
The collected prenatal data included multiple gestations, normal pregnancy and in vitro fertilization and embryo transfer, gestational diabetes mellitus, pregnancy-induced hypertension, clinical and histological chorioamnionitis, administration and completion of antenatal corticosteroid therapy, delivery method, maternal age, and maternal and paternal educational level. The educational level of the parents was classified into two groups according to whether they have graduated from college or not.
The analyzed perinatal data included gestational age, sex, and body measurements (weight and head circumference) at birth. The variables in the delivery room included 1- and 5-minute Apgar scores and implementation of neonatal resuscitation. Respiratory and cardiac statuses in the neonatal intensive care unit (NICU) were investigated as the presence of respiratory distress syndrome and patent ductus arteriosus. Also, the use of steroid therapy and diagnosis and grade of BPD were considered. The diagnosis and severity of BPD were defined by the need for supplemental oxygen support at 28 days of postnatal age and 36 weeks of corrected age [13]. ROP was defined using the international committee criteria, and necrotizing enterocolitis (NEC) was defined as higher than stage II according to modified Bell’s criteria [14]. IVH grade I was defined according to the classification of Papile et al. [15] Culture-proven sepsis, duration (days) of total parenteral nutrition (TPN), and automated auditory brainstem response result were also included in the neonatal variables. The body measurements at the time of NICU discharge were considered.
3. Neurodevelopmental assessment
In the registry, the BSID-II or BSID-III test was performed for VLBW infants depending on the routine procedure in the followup center. In the study, we included infants who underwent the BSID-III test at corrected ages of 18 to 24 months. Cerebral palsy (CP) was defined as a permanent disorder of movement and posture that causes limitations of physical activity that are attributed to nonprogressive disturbances in the fetal or infant brain and graded according to the Gross Motor Function Classification System of Palisano and associates for children aged ≤2 years [16]. Developmental delay was defined as a composite score of ≤85 (≤1 standard deviation [SD]) in each category [17]. Moderate delay was defined as a composite score of ≤70 (≤2 SD), and severe delay was defined as a composite score of ≤55 (≤3 SD).
4. Statistical analysis
The baseline demographic, anthropometric, and clinical characteristics of the study population were described using either the median (interquartile range [IQR]) or numbers of cases (percentage). For categorical variables, the chi-square and Fisher exact tests were used to compare the associations of variables between the normal development and developmental delay groups. The Mann–Whitney U and Wilcoxon rank-sum tests were used to compare continuous variables. To identify the quantitative relationships between variables, analysis was performed in two steps: a univariate analysis and then a multivariate analysis. The univariate logistic regression analysis was employed to identify the variables that showed an apparent association with neurodevelopmental impairment. Then, the multivariate logistic regression analysis was performed to identify the strong predictors for the adverse neurodevelopmental outcomes. In the multivariate analysis, gestational age and birth weight were included in the analysis assessing outcome prediction. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA), and associations were presented as odds ratio (OR) and 95% confidence interval. For all tests, P<0.05 was considered significant.
RESULTS
1. Study population
The selection process of the study population is summarized in Figure 1. During the study period, 5,899 VLBW infants were born and registered in the KNN registry. After discharge, 2,759 (47.4%) of the VLBW infants were followed up in outpatient clinics, and 1,053 VLBW infants (17.8%) underwent the BSID test at corrected ages of 18 to 24 months. Of the 1,053 VLBW infants, 383 (36.3%) underwent the BSID-III test. Of the 383 VLBW infants, 77 infants with abnormal findings in the neurological imaging tests (n=43), IVH grade II or higher (n=25), PVL (n=9), or major congenital malformation (n=8) were excluded. Eventually, 285 VLBW infants who underwent the BSID-III test at corrected ages of 18 to 24 months were included for analysis. The mean gestational age was 29 weeks (IQR, 27 to 30 weeks), and the mean birth weight was 1,130 g (IQR, 900 to 1,290 g) (Table 1). The mean gestational age and birth weight of the remaining group were 28.3 weeks (P=0.06) and 1,074 g (P=0.17), respectively, which did not show statistical significance. Furthermore, three of the enrolled VLBW infants were diagnosed with CP, and the mean discharge weight was 2,470 g (Table 2).
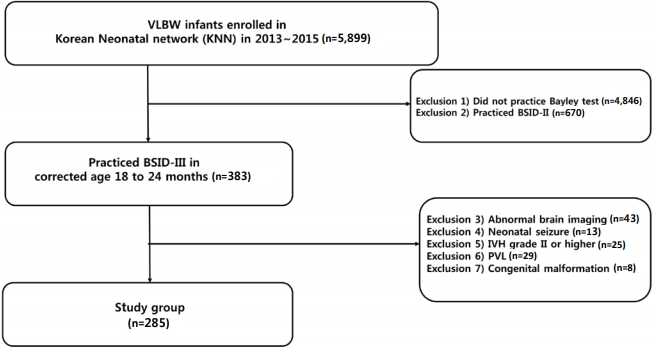
Enrollment of study group. Abbreviations: VLBW, verylow-birth-weight; BSID, Bayley Scales of Infant and Toddler Development; IVH, intraventricular hemorrhage; PVL, periventricular leukomalacia.
2. Neurodevelopmental assessment
The incidence of developmental impairment was highest for language (20.7%, 59/285), followed by cognition (11.9%, 34/285) and motor function (11.2%, 32/285). The mean±SD developmental scores in the cognition, language, and motor scales were 99.99±13.59, 95.14±14.72, and 99.32±11.61, respectively. The average score was the lowest in the language group in both total study and delayed VLBW groups. Moreover, the incidence of moderate and severe delay was the highest in the language scale (Table 3).
3. Analysis for the predictors of adverse neurodevelopmental outcome
In the univariate analysis, cognition delay was significantly associated with multiple factors. Lower 5-minute Apgar score, lower birth weight, moderate and severe BPD, IVH grade I, and longer TPN duration were associated with the poor cognitive outcome (Supplementary Table 1). However, in the multivariate models, none of the factors were significantly related. IVH grade I (P=0.079) and moderate and severe BPD (P=0.056) were highly suspected predictors, and they showed marginal associations (Table 4).

Multivariate Analysis of the Cognitive Outcomes of Preterm Infants at Corrected Ages of 18 to 24 Months (n=285)
In terms of the language delay, birth weight and head circumference at the time of birth and discharge were significant factors associated with the outcome in the univariate analysis (Supplementary Table 2). Also, IVH grade I and paternal educational level were associated with language delay. In the multivariate analysis, the paternal educational level was the only related factor. As the paternal educational level increased, the incidence of language delay decreased (OR, 0.33; P<0.05) (Table 5).

Multivariate Analysis of the Language Outcomes of Preterm Infants at Corrected Ages of 18 to 24 Months (n=285)
In the univariate analysis of motor delay, birth weight, head circumference at birth, and 5-minute Apgar score were significant factors. Similar to other scales, moderate and severe BPD, IVH grade I, total TPN duration, and head circumference at discharge were the major risk factors (Supplementary Table 3). In the multivariate analysis, birth weight and head circumference at discharge were significant factors associated with motor delay (P<0.05) (Table 6).
DISCUSSION
The study analyzed the current incidence of and significant risk factors associated with the poor neurodevelopmental outcome of VLBW infants at corrected ages of 18 to 24 months with BSID-III scores, especially those who did not show major brain injury. After discharge, 47.4% of the VLBW infants were followed up in outpatient clinics, and 17.8% underwent the BSID test at corrected ages of 18 to 24 months. The implementation rate of BSID in South Korea was lower than that of other nations, 79.1% in Switzerland and 74.9% in Canada [6,18]. We insist that the implementation rate of the Bayley tests should be increased for proactive surveillance in VLBW infants.
In our study, 11% to 20% of VLBW infants showed poor neurodevelopmental outcome although the infants with neonatal brain injuries were excluded. Considering that the BSID-III test has a tendency to overestimate infants’ neurodevelopmental status [17,19], the incidence of poor outcome would have been underestimated and may be higher.
Of the three categories in BSID-III, the incidence of language delay was the most prominent. Several studies showed that preterm infants without neurological impairment could have prominent language delay [20], which can persist through school age [21,22]. Therefore, early intervention is necessary, and there has been practical improvement in outcome [23,24]. We emphasize the necessity of early intervention in language delay, even VLBW without evident brain injuries.
Our robust finding was that the paternal educational level was a significant factor associated with language delay in the multivariate analysis. Previous studies showed that socioeconomic status and maternal educational level were relevant environmental factors in developmental delay [4,25,26]. However, to the best of our knowledge, this is the first study to emphasize the association of language delay with the paternal educational level in VLBW infants. Our study is in line with Pancsofar et al. [27] that the paternal educational level significantly contributed to the child’s expressive language development. We could not determine whether the result affected the outcome directly or indirectly as our cohort had no data on the socioeconomic status, family stress factor, and home environment. However, we should emphasize that not only maternal factors but also paternal factors are crucial to language delay.
In our analysis, well known risk factors including ROP and NEC also did not impact the neurodevelopmental outcome in prematurity [28-30]. On the contrary, birth weight and head circumference had significant effects on developmental delay, consistent with previous studies [6]. Among the predictable variables at discharge, BPD showed significant impacts on neurodevelopmental outcome. Previous studies have shown that BPD could have an impact on the brain microstructure such as white matter connectivity and reduction in brain volume especially in the cerebellum and corpus callosum [31,32]. Moreover, its chronic disease entity could adversely affect daily life and social interaction, which is a crucial factor for development. IVH grade I, which is controversial on its impact on delayed outcome, exhibited a marked influence [33-35]. Similar to BPD, a previous study showed that IVH I affects the brain microstructure. It indicates that while VLBW have normal brain MRI findings, neonatal variables could actually impact on its microstructures.
A remarkable finding was that in the study group, three infants were diagnosed with diplegic CP. All of them did not show any signs of neurological abnormalities except IVH grade I. The result indicates that prematurity itself could be a crucial risk factor for CP. Also, it implies that clinicians should carefully observe the development of all VLBW infants, even those without brain injuries.
The strength of the study is that it is based on a large populationbased nationwide cohort. In our knowledge, this is the first study to analyze only VLBW infants without neurological abnormalities with BSID-III. Several limitations of this study need to be mentioned. Although our study is based on a nationwide cohort, the number of the study population was relatively small that we could not validate the prediction model. Also, as mentioned earlier, the implementation rate of the Bayley test was poor that it is unclear whether the result can represent the entire population. In the survey, environmental factors including socioeconomic status, residence, and children day care center were excluded, which could have affected the neurodevelopmental outcome.
In conclusion, approximately 20% of VLBW infants without major brain injury have developmental delay; language delay was the most prominent of the three categories. Factors that can assume developmental delay are BPD higher than moderate, IVH grade I, paternal educational level, birth weight, and head circumference at discharge. We emphasize that even in VLBW infants without brain injury, clinicians should be aware of the risk factors for poor neurodevelopmental outcome.
SUPPLEMENTARY MATERIALS
Supplementary materials related to this article can be found online at https://doi.org/10.5385/nm.2020.27.4.151.
Univariate Analysis of the Cognitive Outcome of the Enrolled Infants
Univariate Analysis of the Language Outcome of the Enrolled Infants
Univariate Analysis of the Motor Outcome of the Enrolled Infants
Notes
Ethical statement
The data registry was approved by the Institutional Review Board as each hospital was a participant in the Korean Neonatal Network (IRB No. 2013-06-025). Informed consent was obtained from all patients through their enrollment in NICUs participating in the Korean Neonatal Network.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Author contributions
Conception or design: J.H.C.
Acquisition, analysis, or interpretation of data: J.H.C., N.C., Y.J.K.
Drafting the work or revising: J.H.C., H.J.L., C.R.K., H.K.P.
Final approval of the manuscript: H.K.P.
Acknowledgements
This research was supported by a fund (2019-ER7103-00#) by Research of Korea Centers for Disease Control and Prevention.




